Table of Contents
Sleep apnea is a serious sleep disorder in which breathing involuntarily stops during sleep. Patients with sleep apnea experience multiple breathing pauses when they sleep. Usually, people with sleep apnea have loud snoring and may gasp for air. The breathing pauses cause poor sleep quality, leading to tiredness during the day and also and it affects the oxygen supply to the body, with serious health consequences.
There are two kinds of Sleep apnea: obstructive sleep apnea and central sleep apnea. Health problems associalted with sleep apnea are like hypertension, diabetes, stroke and dementia.
Obstructive sleep apnea(OSA) has been linked to a number of ocular complications including Floppy eyelid syndrome (FES), Keratoconus, Non-arteritic anterior ischemic optic neuropathy (NAION), Glaucoma, especially normal-tension glaucoma (NTG), and Papilloedema.
Ocular Diseases Linked to Sleep apnea
Floppy eyelid syndrome (FES)
An eye conditions in which a person has a floppy upper eyelid that easily turns outwards (everts). FES patients have eyelids that are loose and rubbery, which can cause problems when they come in contact with the pillow. People suffering from FES experience dry, irritated eyes especially in the morning, which improves as the day goes on.
Almost all of those who have floppy eyelid syndrome have obstructive sleep apnea, although a small minority of all OSA patients have FES. Eye specialists consider floppy eyelids a warning sign of undiagnosed sleep apnea, and may order a sleep study for the patient.
The connection between the two medical conditions hasn’t been completely understood by researchers. Both obstructive sleep apnea and FES share risk factors like obesity and age which could be one of the reasons for this link between the two. Another theory is that OSA patients have greater tissue elasticity and tissue elasticity also has an effect on incidences of FES. FES can be easily identified in patients with obstructive sleep apnea by asking about ocular discomfort symptoms.
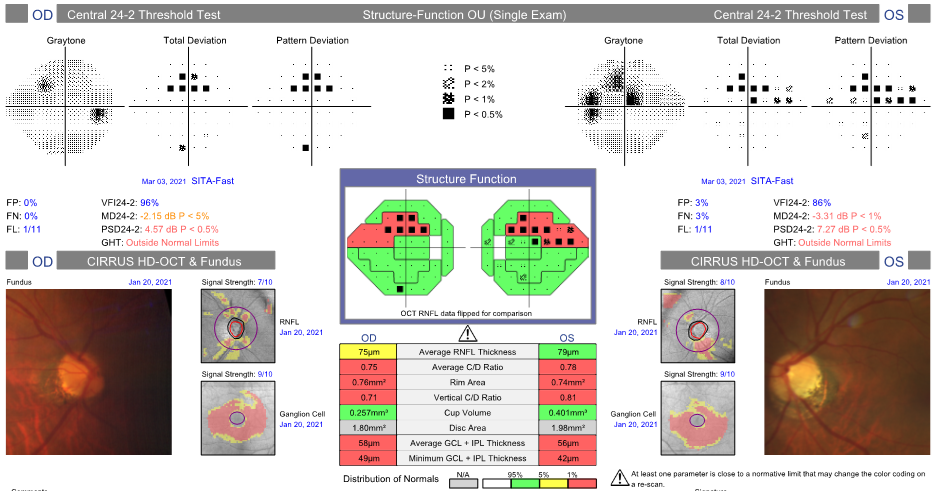
Glaucoma
Glaucoma is the second leading cause of blindness in the world. It is the damage of the optic eye nerve. People with OSA are more likely to suffer from glaucoma. Sleep apnea causes episodes of interrupted breathing which can cause oxidative stress damage to the optic nerve, recurrent hypoxia, and an increase in vascular resistance. OSA has been linked to two types of glaucoma- primary open-angle glaucoma (POAG) and normal-tension glaucoma (NTG).
Numerous studies have been conducted to study the possible link between OSA and glaucoma.
NAION
Non-arteritic anterior ischemic optic neuropathy (NAION) is a painless, sudden, and irreversible loss of vision. NAION occurs because of the loss of blood flow to the optic nerve. There is a greater chance of developing NAION in patients with untreated OSA. Treatment of sleep apnea cannot reverse NAION, however there is a possibility of preventing a NAION attack in the other eye with sleep apnea treatment. Physicians treating OSA can play an important role in preserving the contralateral eye in patients with NAION by alleviating risk factors.
Papilledema
Papilledema is a manifestation and feature of elevated intracranial pressure or idiopathic intracranial hypertension (IIH). Obstructive sleep apnea is commonly associated with brain functional and morphological alterations. Although there have been many cases that show the obstructive sleep apnea and Papilledema together in patients the link between the two is not well known. The American Academy of Ophthalmology has noted that the increase in body carbon dioxide levels because of interrupted breathing from sleep apnea might be one connection between the two.
Dry Eye Syndrome
The least serious but the most common eye conditions that is linked to sleep apnea is dry eyes. Dry eyes can significantly disrupt the quality of life of patients and therefore should also be addressed. CPAP treatment of sleep apnea is one of the major reasons for dry eye syndrome in sleep apnea patients. While the treatment is a blessing for many patients and their problems associated with sleep apnea, the air can leak from the mask and enter the eyes continuously for 8 hours while the person is sleeping. This causes itching, burning, irritation, and watering.
A nasal mask, adjusting the fit of the CPAP mask, or changing sleep position can sometimes provide relief from dry eyes. Preservative-free artificial tear drops or ointments are another way of addressing dry eye syndrome.

Conclusion
There is a strong connection between sleep apnea and vision-threatening ocular conditions. The physiological effects of interrupted breathing, increased intracranial and ocular pressure and inflammation are some of the reasons behind these ocular conditions. Eye doctor can spot connections between these visual conditions and sleep apnea and recommend you to a sleep study and sleep apnea diagnosis. Seeing an eye doctor and conducting eye exams regularly can restore vision, prevent vision loss, and help in diagnosing sleep apnea.