Table of Contents
Our eyes are truly remarkable organs, allowing us to perceive the world around us with incredible precision. But what happens when the left and right eyes don’t quite work in harmony? That’s where eye muscle disorders come into play.
In this article, we will explore some common eye muscle disorders that may necessitate surgical intervention. These conditions, such as simple strabismus, nystagmus, and paralytic strabismus, can significantly impact visual function and eye alignment.
Understanding their specific characteristics and the surgical solutions available is crucial for those affected by these conditions, or those caring for someone who is.
Understanding Eye Muscle Disorders
Eye muscle disorders, also known as strabismus or extraocular muscle disorders, refer to conditions where the muscles responsible for eye movement and alignment do not work in sync. The brain, nerves and eye muscles coordinate the movement of both eyes, allowing them to focus on the same object and maintain alignment. When this complex system malfunctions, it can result in various vision problems, including double vision, reduced depth perception, and a visible misalignment of the eyes.
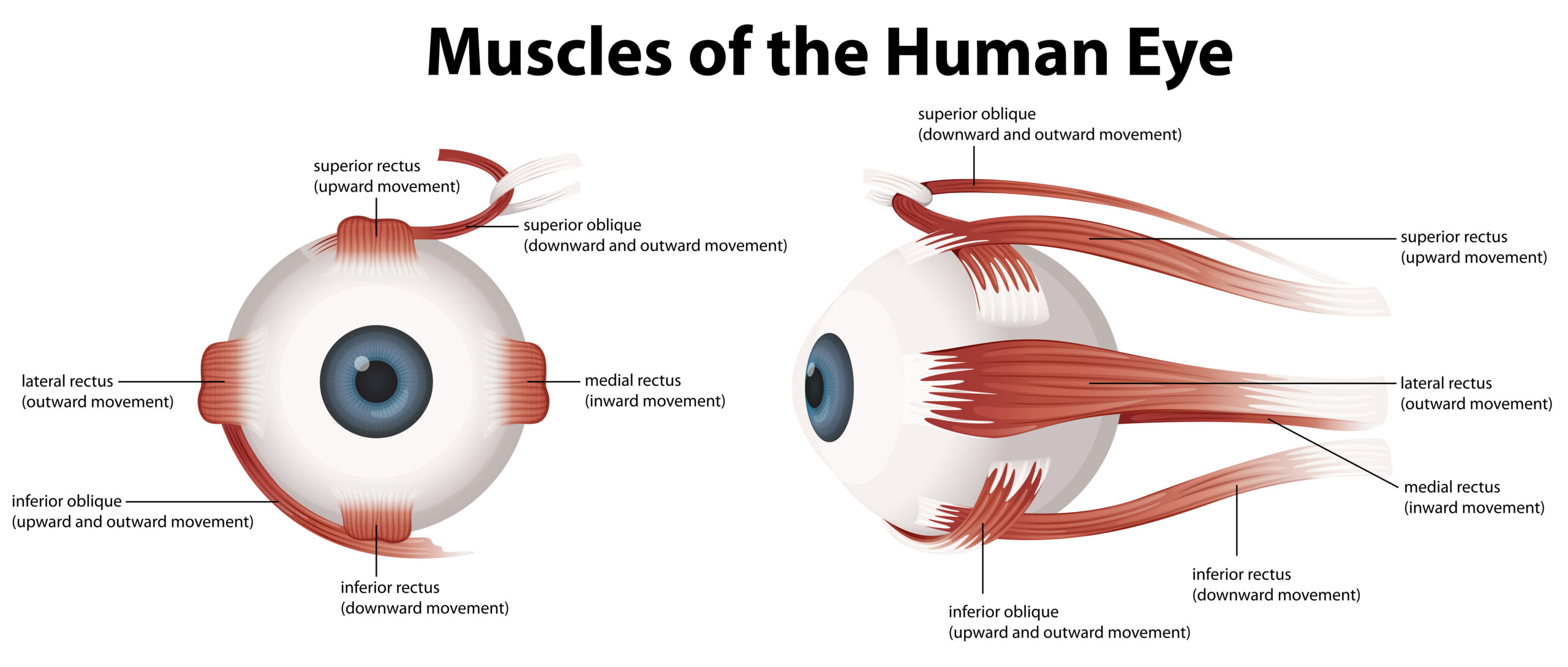
Understanding the basic anatomy of eye muscles is essential. There are six extraocular muscles attached to each eye that control its movements. These muscles work in pairs, with one muscle contracting while the opposing muscle relaxes to move the eye in different directions. The proper functioning of these muscles is crucial for binocular vision, where both eyes work together to provide a single, three-dimensional image of the world.
While some eye muscle disorders may develop due to underlying health conditions or injuries, others can be present from birth. It is important to note that these conditions can affect people of all ages, from infants to adults.
Strabismus – Crossed Eyes
Strabismus, often colloquially referred to as “crossed eyes,” is one of the most common eye muscle disorders. It occurs when the extraocular muscles fail to coordinate correctly, leading to misalignment of the eyes. This misalignment can manifest in different ways:
- Esotropia: In this form of strabismus, one or both eyes turn inward, toward the nose.
- Exotropia: characterised by one or both eyes turning outward, away from the nose.
- Hypertropia: one eye is positioned higher than the other, resulting in vertical misalignment.
Strabismus can have several causes, including problems with the eye muscles, the nerves controlling these muscles, or the brain’s control over eye movements. It can also be related to refractive errors, such as near-sightedness or far-sightedness.
Children and adults with strabismus may experience double vision or amblyopia (lazy eye), which can adversely impact their quality of life.
Nystagmus – Involuntary Eye Movements
Nystagmus is another eye muscle disorder characterised by rapid, involuntary eye movements. These movements can occur in various directions: horizontal (side-to-side), vertical (up-and-down), or even rotational (torsional). Nystagmus can be classified into two main categories:
- Congenital Nystagmus: This type is present at birth or develops during infancy and tends to be stable over time.
- Acquired Nystagmus: Acquired nystagmus develops later in life due to underlying medical conditions, medications, or other factors.
The rapid eye movements associated with nystagmus can make it challenging to maintain steady focus on objects, leading to reduced visual acuity and difficulties with tasks that require visual concentration.
Paralytic Strabismus – Weak Eye Muscles
Paralytic strabismus, also known as paralytic or paretic strabismus, occurs when one or more of the extraocular muscles become weak or paralysed. This weakness can result from damage to the nerves that control the eye muscles or other underlying medical conditions. Paralytic strabismus often leads to limited eye movement and may cause double vision when attempting to look in certain directions.
It is essential to distinguish between paralytic strabismus and non-paralytic strabismus. In non-paralytic strabismus, the eye muscles themselves are typically healthy, but their coordination is impaired. In contrast, paralytic strabismus involves an issue with the muscles themselves, or the nerves controlling them.
Surgical Intervention for Eye Muscle Disorders
When non-surgical treatments, such as eyeglasses, eye patches, or prisms, do not yield the desired results in correcting eye muscle disorders, surgical intervention may be an option. The primary goal of eye muscle surgery is to restore proper eye alignment and coordination. Different surgical techniques are available, depending on the specific disorder and the individual patient factors.
Here are some common surgical approaches:
- Muscle Recession: In this procedure, an eye surgeon weakens a specific eye muscle by detaching it from the eye and reattaching it farther back. This technique is often used to treat strabismus where an eye turns inward (esotropia).
- Muscle Plication: Plication involves shortening a portion of an eye muscle. This procedure is typically used to strengthen eye muscles.
- Adjustable Sutures: Adjustable sutures allow for precise fine-tuning of eye alignment post-surgery. Eye surgeons can make adjustments after the procedure to achieve the desired eye alignment.
These surgical techniques are performed by ophthalmologists who specialise in eye muscle surgery. The choice of technique depends on the patient’s specific condition and the surgeon’s expertise and experience.
Preparing for Eye Muscle Surgery
Preparation for eye muscle surgery is a crucial step in ensuring the best possible outcome. Patients will typically undergo a thorough preoperative evaluation to assess their eye health, determine the appropriate surgical approach, and address any underlying conditions. The evaluation may include vision tests, eye examinations, and discussions with the surgeon about treatment goals and expectations.
Anaesthesia options will also be discussed with the surgeon. Depending on the patient’s age and medical condition, either general anaesthesia or local anaesthesia with sedation may be recommended for the procedure. The surgeon will explain the chosen anaesthesia method and any associated risks.
Understanding what to expect on the day of surgery is vital for reducing anxiety and ensuring a smooth experience. Patients should receive clear instructions about fasting, medications, and any specific preparations they need to make.

Recovery and Rehabilitation
After eye muscle surgery, the postoperative period is essential for recovery. Eye drops are prescribed for a short duration, and it is important to keep the eyes dry and not to rub the eyes. Recovery timeframes can vary, but patients may experience some discomfort initially. Follow-up appointments are vital to assess the surgical outcome and make any necessary adjustments. In some cases, non-surgical rehabilitation may be recommended to optimise results.
Conclusion
Eye muscle disorders, such as simple strabismus, nystagmus, and paralytic strabismus, can have a profound impact on vision and eye alignment. Surgical intervention is often necessary to address these conditions effectively. By understanding the characteristics of these disorders and the available surgical solutions, individuals can make informed decisions about their eye health. If you or someone you know is experiencing symptoms of an eye muscle disorder, don’t hesitate to seek professional advice. Early intervention can lead to better outcomes and an improved quality of life.
Dr Parth Shah is an ophthalmologist in Canberra who is committed to providing excellent surgical care to all of his patients. He implements modern research and technology in order to achieve optimal outcomes.











