Table of Contents
What is strabismus (squint)?
Strabismus (also known as squint) is a common eye problem in children and adults. It refers to a misalignment of the two eyes. Some people may also call it a “lazy eye” or an “eye turn”.
Strabismus has a significant functional and psychosocial impact on people, and it can be treated. Dr Parth Shah has experience in treating all types of strabismus, including performing eye muscle surgery. He developed this specialised expertise and surgical skill by working with world-renowned specialists at centres in Australia, the UK, and the USA.
Dr Parth Shah performs eye muscle surgery for children and adults.
Types of strabismus: Esotropia, Exotropia, Hypertropia, Hypotropia
Strabismus can be intermittent or constant. The terminology used to describe the strabismus is based on the direction of the misaligned eye.
- A convergent misalignment (inward turn) is an esotropia.

Causes: Esotropia can result from issues with the eye muscles, neurological problems, or refractive errors. It may also be associated with farsightedness (hyperopia).
Treatment: Treatment options for esotropia may include corrective lenses, eye patches, eye exercises, or in some cases, surgical intervention to adjust the eye muscles.
- A divergent misalignment (outward turn) is an exotropia.

Causes: Exotropia can be associated with muscle imbalances, vision problems, or issues with the eye-brain connection.
Treatment: Treatment approaches may include corrective lenses, eye exercises, and surgery to align the eyes properly. The choice of treatment depends on factors such as the severity of the condition and the age of the individual.
- When the eye is higher than the other, it is a hypertropia.

Causes: Hypertropia may stem from imbalances in the vertical muscles of the eyes, nerve issues, or other underlying conditions affecting eye movement.
Treatment: Treatment options include corrective lenses, prisms, or surgery to adjust the eye muscles and correct the vertical misalignment.
- When the eye is lower than the other, it is a hypotropia.

Causes: Similar to hypertropia, hypotropia can result from imbalances in the eye muscles or underlying neurological conditions affecting eye movement.
Treatment: Treatment approaches may include corrective lenses, prisms, or surgical intervention to address the underlying muscle imbalances and align the eyes vertically.
Most forms of intermittent strabismus can become more apparent in certain situations, e.g. fatigue, illness or intoxication.
Signs and Symptoms of Strabismus
When the eyes are misaligned and looking in different directions, double vision can result. Infants and children with strabismus can ignore (“suppress”) the double image because the brain is able to adapt to the misalignment. However, these children will not develop normal “binocular” or “3-D” vision, as their brain did not learn to use both eyes together. Gross and fine motor development can be reduced. Children with strabismus can start to favour one eye over the other (amblyopia), which needs to be monitored and treated.
Adults with new strabismus can suffer debilitating symptoms:
- Double vision
- Visual confusion
- Eye “strain” and headache
- Reduced field of vision
- Neck pain from turning or tilting the head to avoid double vision
There are many negative psychosocial impacts of strabismus on daily interaction. Studies have demonstrated that patients with strabismus have a reduced quality of life. Children can be bullied at school due to the appearance. Adults with strabismus can experience reduced self-esteem, and difficulties with social interactions both socially and professionally. This is because it can seem like they are not maintaining eye contact when one eye drifts in or out.
Myths & Facts about Strabismus (squint)
Myth 1: Squint in small children can go away on its own
Fact 1: A newborn and young infant until six months of age can have an intermittent squint. After this age, it is uncommon for a squint to disappear on its own. This is a popular belief harboured by many parents and re-enforced by some doctors too. In older children, a delay in diagnosis and treatment could potentially lead to reduced vision in the child. Any constant strabismus should be evaluated by a paediatric ophthalmologist.
Myth 2: Squint is just a cosmetic problem
Fact 2: In addition to strabismus being an issue with appearance, it is often also a significant functional problem. This is because a squint can lead to reduced vision (amblyopia) and reduced field of vision. Early treatment of squint may be recommended to prevent deterioration of vision and binocularity – not only to straighten the eyes for reconstructive reasons.
Myth 3: There is no good treatment for squint
Fact 3: Depending on the type of squint, there are many treatment options like glasses, prisms and eye muscle surgery. Any one or a combination of these treatment modalities may have to be used depending upon the case. Treatment of squint may be long term and generally associated with successful results. Squint can be treated at any age, even in adults.
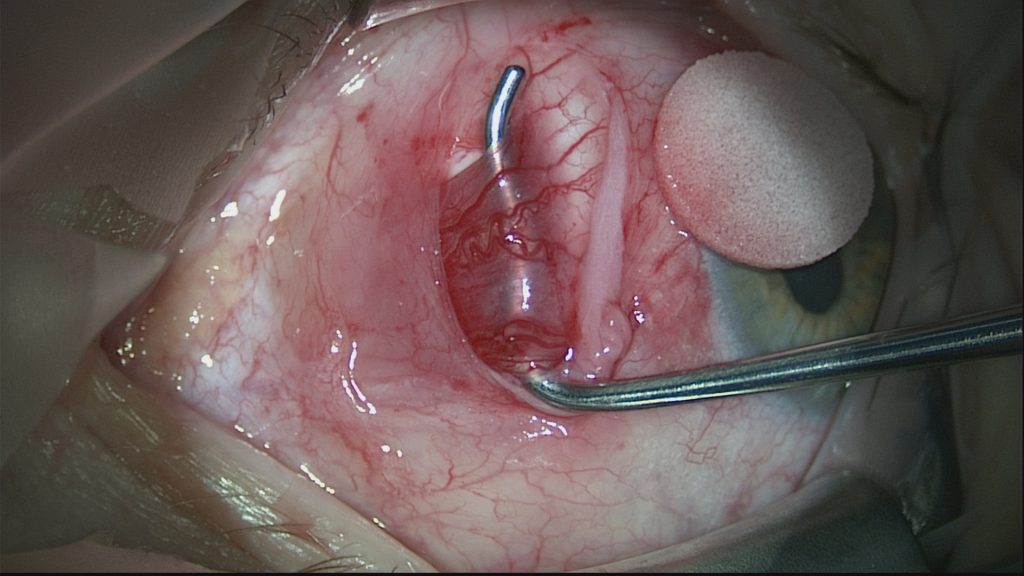
Myth 4: Squint surgery will cause damage to the eye
Fact 4: Eye muscle surgery is generally very safe. It is an extraocular procedure, i.e. it does not involve opening or entering the eye like in cataract surgery. The extraocular muscles on the white of the eye (sclera) are weakened, strengthened or moved to a different location. An eye surgeon will discuss the specific risks and benefits for each individual patient.
Myth 5: Squint will recur after surgery
Fact 5: This is a common fear in patient’s and parents’ minds, and prevents them from going in for the surgery in the first place. If eye muscle surgery is recommended, the risks of recurrence are outweighed by the benefits to the patient. Recurrence may occur may occur months or years after surgery, and there may be non-surgical and surgical options to treat this.
Causes of Strabismus
There are many possible causes of strabismus:
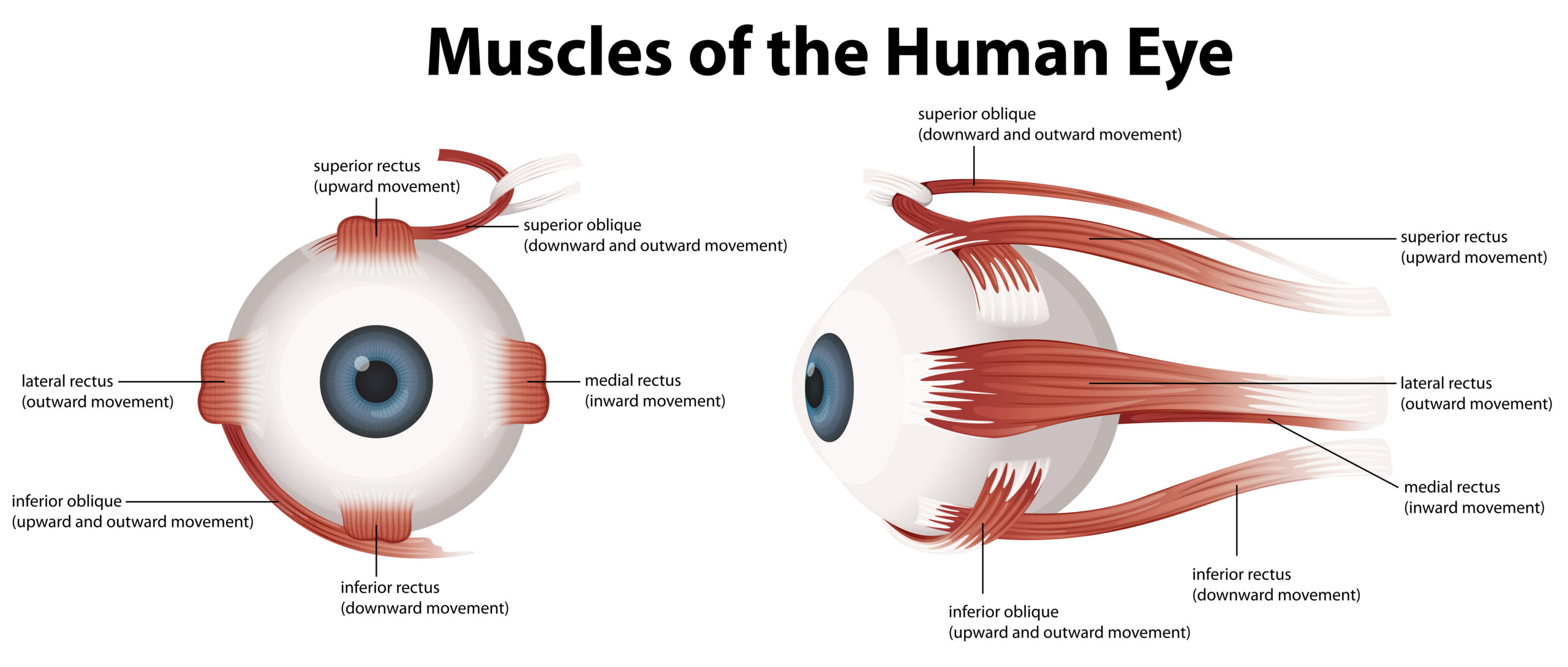
- Muscle Imbalance: The most common cause of strabismus is an imbalance in the muscles that control the movement of the eyes. If one eye’s muscles are weaker or stronger than the other, it can lead to misalignment.
- Refractive Errors: Uncorrected refractive errors, such as nearsightedness, farsightedness, or astigmatism, can contribute to strabismus. When the eyes struggle to focus properly, it may lead to misalignment.
- Childhood Development: Strabismus can develop in childhood, often due to problems with the development of the eye muscles or the brain’s control of these muscles.
- Genetic Factors: There is evidence to suggest that a family history of strabismus may increase the likelihood of a person developing the condition. Genetic factors may contribute to muscle imbalance or other structural issues.
- Neurological Conditions: Certain neurological disorders or injuries to the brain can affect the control of eye movements, leading to strabismus.
- Amblyopia (Lazy Eye): Strabismus can sometimes lead to amblyopia, where the brain favours one eye over the other. This can further exacerbate the misalignment.
- Premature Birth: Babies born prematurely may be at a higher risk of developing strabismus, possibly due to incomplete development of the eye muscles or the visual system.
- Medical Conditions: Certain medical conditions, such as Down syndrome or cerebral palsy, may be associated with an increased risk of strabismus.
- Eye Injuries or Trauma: Physical injuries to the eye or head trauma can damage the eye muscles or the nerves controlling eye movement, leading to strabismus.
- Issues Affecting the Eye Socket: Problems affecting the eye socket, such as a fracture or thyroid orbitopathy (Graves disease), can lead to strabismus due to eye muscle imbalance.
It is important to note that the exact cause of strabismus can vary from person to person, and in some cases, the cause may not be easily identified. Early detection and treatment are crucial for managing strabismus, and interventions may include corrective lenses, eye patches, or surgery to realign the eyes.
Diagnosis and Treatment of Strabismus
Strabismus diagnosis involves a comprehensive eye exam by a professional, inclusive of measuring visual acuity and assessment of ocular alignment and movements. Your doctor will also assess for the presence of a “refractive error” and evaluate the coordination of the eyes, through binocular vision testing. General eye health and patient history provide your doctor with context around which the strabismus has developed.
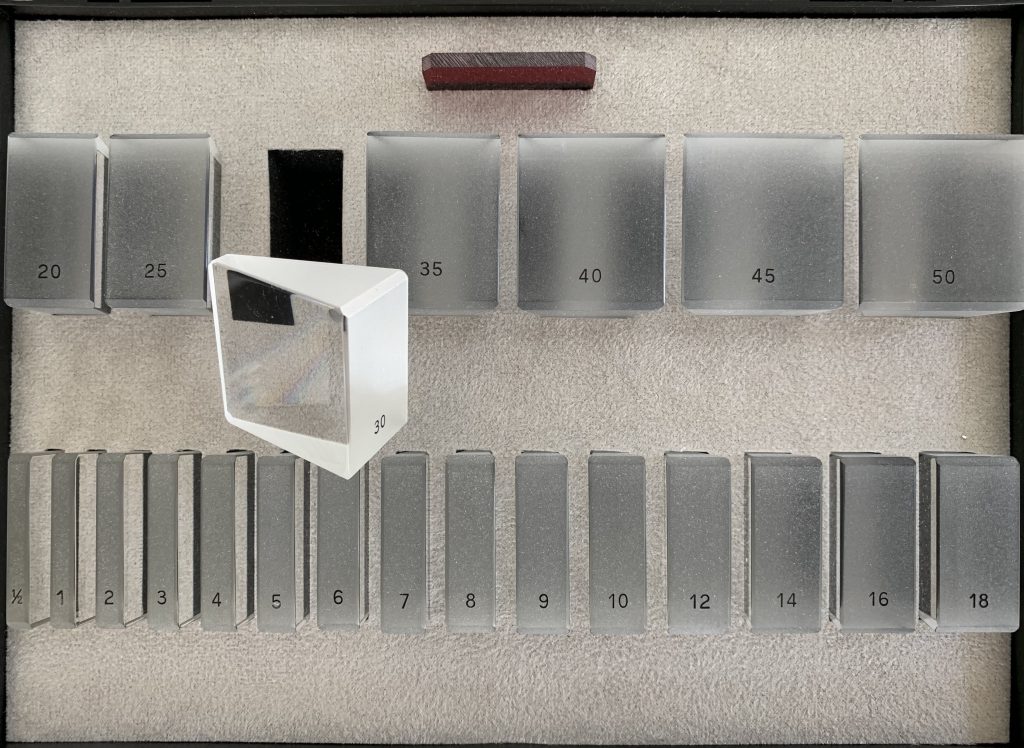
The type and size of the strabismus is measured accurately using prisms and instruments for checking binocular (“3-D”) vision.
The best treatment option will depend on a number of factors including patient symptoms, age, underlying diagnosis and previous treatment.
- Management of Reversible Disease Processes: Any reversible disease process needs to be managed appropriately, e.g. cataract surgery or treatment of thyroid overactivity (Graves disease).
- Simultaneous Management in Children: In children, focusing error and amblyopia need to be managed simultaneously with the strabismus. Glasses and patching may be necessary.
- Prism Lenses: Incorporation of prism into glasses may be suitable in some types of small angle strabismus in adults experiencing double vision.
- Botulinum toxin: It can be injected directly into an extraocular muscle to induce temporary paralysis. It is used in the treatment of strabismus where surgery is contraindicated, or in situations where future improvement is predicted.
- Spectacles: In some cases, strabismus may be corrected with prescription spectacles. Glasses can help improve focusing and reduce eye strain, especially in cases where refractive errors contribute to the misalignment.
- Eye exercises: Eye exercises and activities designed to improve eye coordination and strengthen the eye muscles.
- Eye Patching: If one eye is significantly weaker, patching the stronger eye may encourage the weaker eye to strengthen and improve coordination. This method is often used in children.
- Eye muscle surgery: Eye muscle surgery can be performed for functional or reconstructive purposes. The muscles are permanently weakened, strengthened or moved to a different position. Surgery is not a final or last resort treatment option for strabismus.
- Combination of Treatments: Depending on the specific case, a combination of treatments may be recommended. For example, a person may undergo surgery and then follow up with eye exercises for optimal results.

Conclusion
Strabismus does not have to limit your vision or your life. Early diagnosis and treatment can significantly improve your eye alignment and overall well-being. If you suspect you or your child might have strabismus, don’t hesitate to seek professional help.
Contact us today for personalised strabismus treatments that can help you.
Author Bio
Dr Parth Shah is an ophthalmologist in Canberra, specialising in cataract and eye muscle surgery. With extensive training and experience, he is renowned for his expertise in the field. Dr Shah is dedicated not only to performing successful surgeries but also to patient education. His compassionate approach, combined with technical proficiency, has earned him the trust and gratitude of countless patients. He is a true advocate for eye health and a trusted name in the Canberra ophthalmology community.