Table of Contents
What is Macular Degeneration?
Macular Degeneration, also known as Age-related Macular Degeneration (AMD) is a painless eye condition that may lead to vision loss. It is an eye disease that is considered a leading cause of loss of vision in people over 60 years of age, often more than glaucoma and cataract. At the present moment, it is considered to be an incurable disease.
The macula is a small are located in the centre of the retina, in the back of the human eye. It is caused when the macula deteriorates, leading to loss of the central vision. Central vision refers to the picture you get when you are looking straight ahead of yourself. On the other hand, peripheral vision is the picture that can be seen from the side of the eye when you are looking straight ahead of yourself.
What are the stages of macular degeneration?
- Early: No symptoms, but an eye doctor can see tiny deposits (drusen) under the macula.
- Intermediate: Some may experience mild central vision blur, especially in low light.
- Advanced: Significant vision loss in the centre. Two forms, which are discussed in more detail below:
- Dry: Light-sensitive cells deteriorate and die (“geographic atrophy”).
- Wet: Abnormal blood vessels leak fluid or bleed, causing distortion and vision loss.
Early detection is key for managing AMD. See an eye doctor regularly.
Types of Macular Degeneration
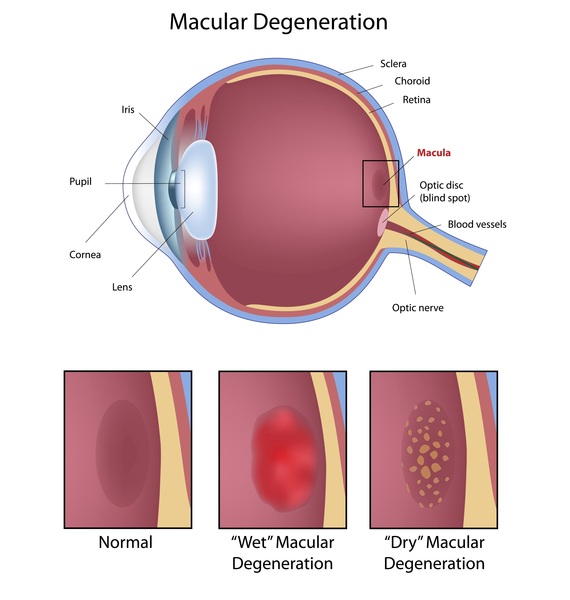
Macular Degeneration is of two types:-
Dry: Dry macular degeneration happens when the tiny yellow deposits develop under the macula. These deposits are known as drusen. About 85 to 90 percent of people who have been diagnosed to be suffering from the disease have dry macular degeneration.
Wet: The remaining 10 to 15 percent of the population with the disease have wet macular degeneration. In wet AMD, abnormal new blood vessels tend to develop under the macula and the retina. The development of these blood vessels is abnormal and affects the vision of the individual through leakage of fluid under and into the retina, and sometimes frank bleeding.
However, it must be noted that an individual can develop both dry and wet types of AMD. The disease may impact either one or both the eyes, and the progression may be slow or rapid. The majority of the cases see the advances in the dry disease without it turning into wet AMD. If the disease is detected early and treatment is started, the disease may not develop into an advanced form.
Symptoms of Macular Degeneration

AMD is considered to be an incurable and progressive eye condition. This means that with time, the condition is likely to get serious. As far as this eye condition is concerned, problems in vision are not noticeable in the early stages of AMD. Also, changes may occur in both eyes simultaneously, but even such changes may not be easily noticeable. Therefore, it is important to be aware of the signs and symptoms of macular degeneration.
Symptoms of both wet and dry macular degeneration vary with a few common symptoms. It has been observed that wet macular degeneration is more rapidly progressive as compared to dry macular degeneration.
Some symptoms of dry macular degeneration are:-
- Reduced central vision
- Distorted straight lines in the field of vision
- Need to have more light or illumination in the room
- Difficulty in adapting to low illuminated areas
- Blurred vision
- Difficulty in face recognition
Some symptoms of wet macular degeneration are:-
- Blurry or dark spot in the field of vision
- Hazy vision
- Rapidly worsening symptoms
Some common symptoms in wet and dry macular vision include reduction in central vision and distortion in images.
Macular Degeneration Risk Factors
Certain factors tend to increase the risk of developing AMD. These factors include:-
- Older age
- Smoking
- Family history
- Comorbid conditions such as cardiovascular disease.
- Overweight individuals.
- Individuals with high cholesterol.
- Sunlight exposure.
- Caucasian ethnicity.
- Gender (slightly higher risk in women).
Macular Degeneration Diagnosis
People are advised to have regular eye check-ups even if their vision is perfectly normal. However, in case of any sudden vision changes, you must visit your eye specialist immediately. Your doctor may conduct certain tests to diagnose the disease.
Very common practice includes dilating the eyes by using eye drops. The doctor then checks for any signs of blood, yellow deposits, or fluids at the back of the eye. Some other tests to diagnose AMD are Amsler Grid Test, Fluorescein angiography, Indocyanine green angiography, and Optical Coherence Tomography.
Treatment for Macular Degeneration
Treatment depends on the type of AMD diagnosed in the patient.
For Dry Macular Degeneration:
- Dietary Supplements: Consumption of vitamins and antioxidants to support eye health and may slow progression.
- Lifestyle Modifications: Including a healthy diet rich in leafy greens, fish, and fruits, and avoiding smoking to reduce risk of progression.
- Low Vision Aids: Devices such as magnifiers, telescopic lenses, and electronic reading systems to help cope with reduced vision for daily activities.
For Wet Macular Degeneration:
- Anti-VEGF therapy: Injection of medications into the eye (intravitreal injections) to control the leakage and growth of abnormal blood vessels under the retina.
- Laser Therapy: Use of laser to seal leaking blood vessels or destroy abnormal blood vessel growth.
- Photodynamic Therapy (PDT): Injection of a light-sensitive drug followed by activation with laser light to destroy abnormal blood vessels.
- Lifestyle Modifications: Same as for dry macular degeneration to support overall eye health and reduce risk factors.
- Regular Eye Exams: Monitoring of macular degeneration progression and adjustment of treatment plan by an eye care professional.
These treatments aim to manage symptoms, slow progression, and preserve vision for individuals with macular degeneration, depending on the type and stage of the disease.
What questions should you ask your healthcare provider in case of macular degeneration?
- What type of macular degeneration do I have, and what stage is it in?
- What are the treatment options available for my condition?
- What are the potential risks and benefits of each treatment option?
- How often should I undergo eye exams to monitor the progression of macular degeneration?
- Are there any lifestyle changes I can make to help manage my condition?
- Are there any dietary supplements or vitamins that may benefit my eye health?
- What symptoms should I watch out for that may indicate a worsening of my condition?
- Are there any low vision aids or devices that could help me manage reduced vision?
- Should I be concerned about any other health conditions or medications that may affect my macular degeneration?
- Are there any clinical trials or research studies that I may be eligible to participate in?
These questions can help you better understand your condition, treatment options, and management strategies for macular degeneration. It’s important to have open and honest communication with your healthcare provider to ensure you receive the best possible care.
Conclusion
Macular Degeneration is a disease with no permanent cure, and by the time you realise it, the disease may have progressed to serious levels. Therefore, it is essential to get your eye check-up done regularly to avoid any unwanted medical issues in the future.
FAQs
1. How can I prevent age-related macular degeneration?
Although there are genetic factors associated with developing age-related macular degeneration (AMD), you can implement diet and lifestyle changes to support macular health. This is inclusive of, maintaining a balanced diet rich in antioxidants, vitamins, and omega-3 fatty acids, avoiding smoking, protecting your eyes from UV light, managing conditions like high blood pressure and high cholesterol, exercising regularly, attending routine eye exams, limiting alcohol intake, and practicing overall healthy living with sufficient sleep and stress management.
2. How long before macular degeneration causes blindness?
The progression of macular degeneration varies, and not everyone with the condition will experience blindness. In some cases, it progresses slowly over many years, while in others, it may lead to severe vision loss more rapidly, especially if untreated. Regular eye exams and following treatment recommendations are crucial for managing macular degeneration and reducing the risk of blindness.
3. What foods should be avoided with macular degeneration?
Limit foods high in saturated and trans fats, processed foods, high-glycaemic index foods, excessive alcohol, and sodium. Avoid nutrient-poor foods and focus on a balanced diet rich in fruits, vegetables, lean proteins, whole grains, and healthy fats to support eye health and manage macular degeneration effectively. Consulting a healthcare provider or dietitian for personalised recommendations is advisable.
4. Can fasting help macular degeneration?
There is limited evidence to suggest that fasting directly helps macular degeneration. While some studies explore benefits of calorie restriction and intermittent fasting for overall health, their specific effects on macular degeneration are unclear. Maintaining a healthy diet rich in nutrients may support eye health, but consult a healthcare provider before making dietary changes.
5. Are there any eye drops for macular degeneration?
As of now, there are no eye drops specifically approved for the treatment of macular degeneration. While several eye drops are available for conditions such as dry eye or glaucoma, they do not directly target the underlying mechanisms of macular degeneration.
6. How long is treatment for macular degeneration?
The duration of treatment for macular degeneration varies depending on several factors, including the type of macular degeneration, the stage of the disease, and the individual’s response to treatment.
Author Bio
Dr Parth Shah is an experienced ophthalmologist in Canberra. With extensive training and experience, he is renowned for his expertise in the field. Dr Shah is dedicated not only to performing successful surgery but also to patient education. His compassionate approach, combined with technical proficiency, has earned him the trust and gratitude of countless patients. He is a true advocate for eye health and a trusted name in the Canberra ophthalmology community.