Table of Contents
Ocular rosacea is a common but often overlooked subtype of rosacea, a chronic skin condition that affects the face. It is a common condition that affects millions of people worldwide. In this article, we will discuss the causes, symptoms, and treatment options for ocular rosacea.
Who is commonly affected by Ocular Rosacea?
- Adults aged 30 to 60.
- Individuals with fair skin.
- More prevalent in women than men.
- Those with a family history of rosacea.
Symptoms of Ocular Rosacea:
The symptoms of ocular rosacea can vary from person to person, but may include:
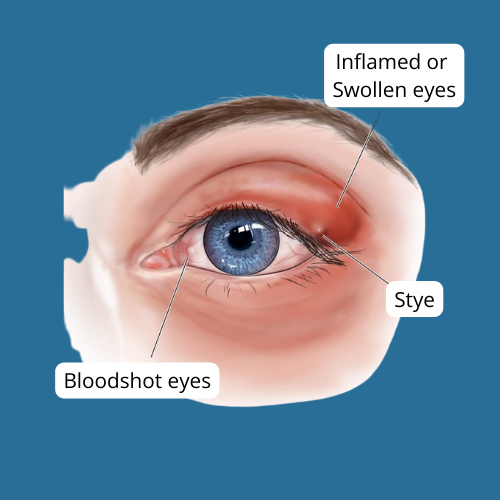
● Redness and swelling of the eyelids
● Recurrent eye or eyelid infections, such as conjunctivitis, blepharitis, styes or chalazion
● A gritty or burning sensation in the eyes
● Dry eyes
● Blurred vision
● Sensitivity to light
● Crusty, flaky eyelids
● Visible blood vessels on the whites of the eyes
It is important to note that not all individuals with ocular rosacea will have skin symptoms of rosacea.
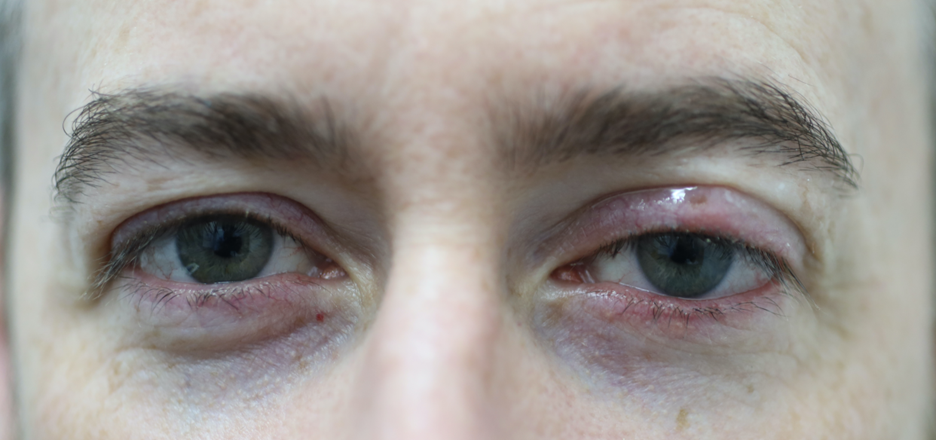
A patient with features of ocular rosacea including red swollen eyelids and a small chalazaion affecting the left upper eyelid.
Causes of Ocular Rosacea:
- Cause: The precise cause of ocular rosacea remains elusive, but it’s thought to result from a blend of genetic predisposition and environmental influences.
Ocular rosacea involves inflammation of the eyelid margins and obstruction of oil glands, leading to irritation and discomfort. - Association with Acne Rosacea: While the direct cause is uncertain, ocular rosacea often coexists with acne rosacea, characterised by facial redness, acne-like bumps, and visible blood vessels.
- Aggravating factors: Aggravating factors such as consuming hot or spicy foods, drinking alcohol, sunlight, wind, or extreme temperatures exposure, emotions like stress, anger, or embarrassment, strenuous physical activities and using hot baths or saunas.
What complications can arise from ocular rosacea?
Complications that may arise from ocular rosacea include potential impact on the cornea, particularly in the presence of dry eyes. These can lead to visual symptoms and issues. Additionally, inflammation of the eyelids (blepharitis) may result in further complications to the cornea, such as irritation caused by misdirected eyelashes. Ultimately, these corneal complications can potentially progress to vision loss.
How is Ocular Rosacea diagnosed?
Ocular rosacea diagnosis typically doesn’t involve complex tests. Doctors rely on:
- Examining your eyes and eyelids: They will check for redness, swelling, inflammation, and other signs.
- Discussing your symptoms: Burning, dryness, foreign body sensation, and light sensitivity are all common.
- Your medical history: Having facial rosacea increases the chance of ocular rosacea.
In some cases, additional tests might be used to rule out other conditions with similar symptoms, but a definitive test for ocular rosacea doesn’t exist.
Treatment Options for Ocular Rosacea:
While there is no cure for ocular rosacea, there are several treatment options that can help manage the symptoms. These include:
Warm compresses: Applying a warm compress to the eyes can help relieve symptoms of dryness and irritation by improving the function of the meibomian glands.
Eyelid hygiene: Keeping the eyelids clean by using a gentle cleanser can help reduce inflammation and prevent infections.
Artificial tears: Over-the-counter artificial tears can help lubricate the eyes and reduce dryness.
Medications: In some cases, medications such as antibiotics, steroids, or immunomodulators may be prescribed to reduce inflammation and manage symptoms.
In addition to these treatments, it is important to avoid triggers that can exacerbate symptoms, such as sunlight, red wine and spicy foods.
When to see a doctor
If you experience persistent redness, irritation, blurry vision, sensitivity to light, discomfort, dryness, swelling, or recurrent infections in your eyes or eyelids, it is essential to consult a doctor. These symptoms may indicate ocular rosacea or related complications, requiring medical attention from a healthcare professional such as an ophthalmologist or dermatologist.
What questions should I ask my doctor?
When visiting your doctor, it is important to ask the following questions:
- What treatments do I need for my condition?
- Will I need to take any medications, and if so, what are they for?
- Do I need to consult a specialist for further evaluation or treatment?
- Are there specific activities, foods, or drinks that I should avoid to support my health and recovery?
Asking these questions will ensure you have a clear understanding of your medical condition and the necessary steps to take for your well-being.
What can individuals do to prevent flare-ups and manage Ocular Rosacea-induced dry eye?
To prevent flare-ups of Ocular Rosacea-induced dry eye and manage the condition effectively, individuals can follow these recommendations:
1. Regularly clean your eyelids with warm water or a doctor-recommended product to keep them free from debris and bacteria.
2. Avoid using makeup, especially during periods of eye inflammation, as it can exacerbate the symptoms. If you do wear makeup, choose non-oily and fragrance-free products.
3. During flare-ups, refrain from wearing contact lenses to reduce irritation.
4. Identify and avoid triggers that worsen your ocular rosacea. Common triggers include alcoholic beverages and spicy foods, which can dilate blood vessels in the face and lead to flare-ups.
Conclusion
Ocular Rosacea is a chronic eye condition that affects the eyes and can cause discomfort and blurry vision. Mild cases of Ocular Rosacea can be managed with self-care measures, but more severe cases may require prescription medications. If you suspect you have Ocular Rosacea, it is important to see an eye doctor to get an accurate diagnosis and proper treatment.
FAQs
Can Ocular Rosacea be cured?
Is Ocular Rosacea contagious?
Can Ocular Rosacea cause blindness?
Are there any known connections between skin rosacea and ocular rosacea?
What are the potential consequences of eyelid scarring due to untreated severe Ocular Rosacea?
How can severe Ocular Rosacea impact the cornea if left untreated?
How common is Ocular Rosacea?
Can you live a normal life with Ocular Rosacea?
Author Bio
Dr Parth Shah is an experienced ophthalmologist in Canberra, specialising in cataract surgery. With extensive training and experience, he is renowned for his expertise in the field. Dr Shah is dedicated not only to performing successful surgeries but also to patient education. His compassionate approach, combined with technical proficiency, has earned him the trust and gratitude of countless patients. He is a true advocate for eye health and a trusted name in the Canberra ophthalmology community.